Written by Kylie Lucas, Pharmacist.
Imagine a world without antibiotics. Minor infections could become serious, life-threatening issues. Some surgical procedures may no longer be possible. The very young, the very old and those with conditions such as cystic fibrosis, cancer or organ transplants would be particularly vulnerable.
Modern medicine has come a long way since the first antibiotic, Penicillin, was discovered in 1928 and began to be used therapeutically in the 1940s. Antibiotics have enabled us to make advances in many fields of health and medicine and achieve a greater life expectancy. However, with time and widespread use of these drugs, resistant bacteria are becoming a major concern and are having a big impact on people who are unfortunate enough to develop resistant types of infections.
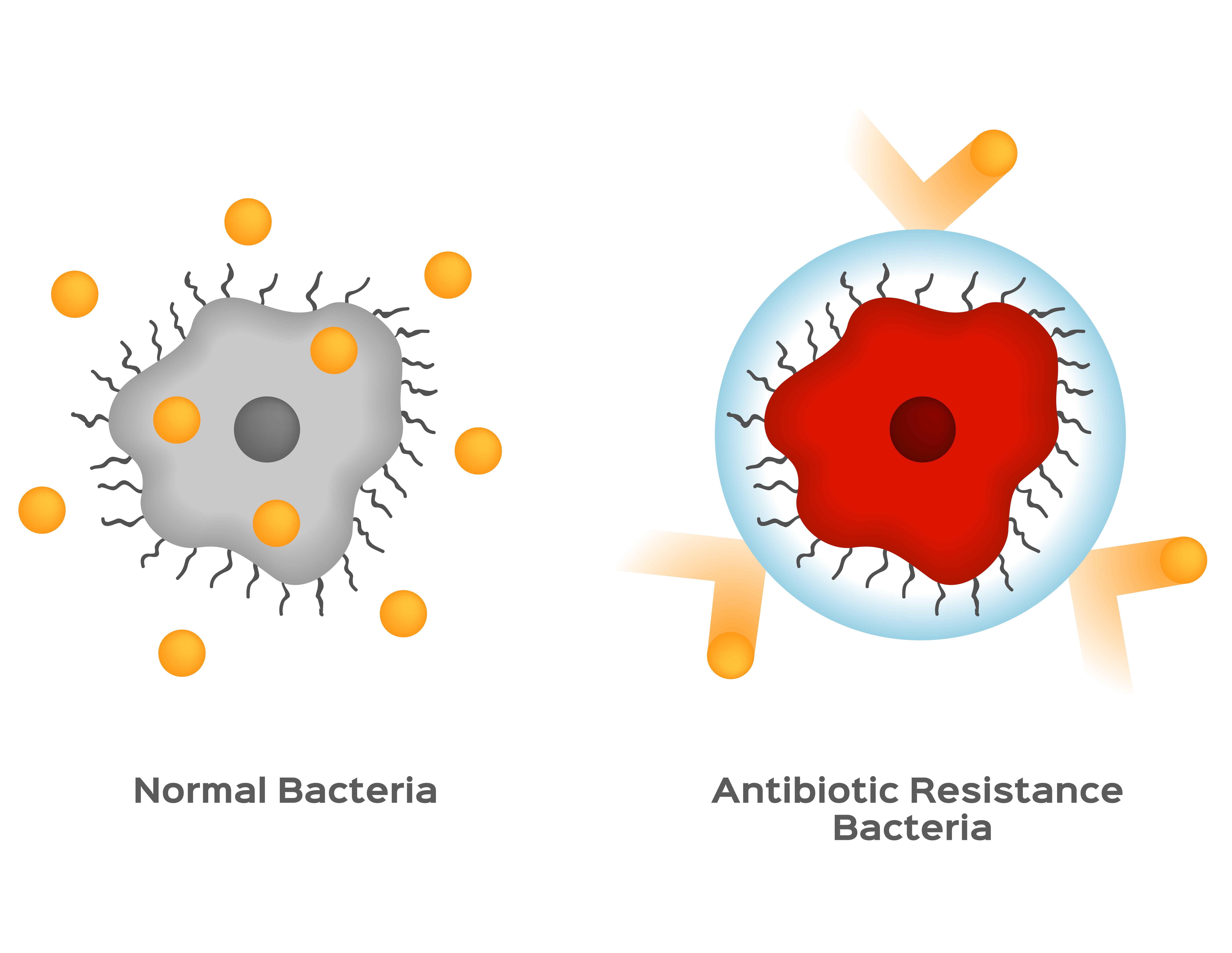
What is antibiotic resistance?
Antibiotics are used to treat bacterial infections. Some strains of bacteria are naturally resistant to certain antibiotics. Other bacteria can adapt to develop resistance after exposure to an antibiotic. Bacteria are able to change so that they are no longer susceptible to the antibiotic’s action. When this happens, the antibiotic will no longer work against that type of infection.
 You may have heard of some cases of antibiotic resistance within your network of friends and family. For example, a person may have complications after a standard surgical procedure such as a knee replacement if they are exposed to bacteria such as Methicillin-resistant Staphylococcus aureus (also known as MRSA, a type of “golden staph”). Or perhaps you know someone who had to take two different types of antibiotics before their urinary tract infection was cured. Antibiotic resistance is a very real problem, affecting Australians in hospitals and in the wider community.
You may have heard of some cases of antibiotic resistance within your network of friends and family. For example, a person may have complications after a standard surgical procedure such as a knee replacement if they are exposed to bacteria such as Methicillin-resistant Staphylococcus aureus (also known as MRSA, a type of “golden staph”). Or perhaps you know someone who had to take two different types of antibiotics before their urinary tract infection was cured. Antibiotic resistance is a very real problem, affecting Australians in hospitals and in the wider community.
What can you do to slow the spread of antibiotic resistance?

Of course, there are many occasions when treatment with antibiotics will be absolutely necessary – and you should always follow your doctor’s advice. Sensible and appropriate use of these important medications will help ensure their effectiveness in the years to come. Remember that your local pharmacist is available to help with any questions or concerns you may have about this subject.
This post was written by Kylie Lucas. Kylie has been a pharmacist for over 10 years and works in a country town pharmacy in the south west of Western Australia. She lives on a farm with her husband, daughter and lots of pet animals.
These Stories on Medication Management
Suite 2 Level 7, 500 Bourke Street
Melbourne, Victoria 3000
Australia
Email us: support@medadvisor.com.au
MedAdvisor is an affiliate member of the World Pharmacy Council.
No Comments Yet
Let us know what you think